Introduction: The Birth of a New Discovery
The Gemma model cancer therapy pathway marks a groundbreaking step in how artificial intelligence can reshape cancer treatment.
In October 2025, Google DeepMind announced that its Gemma family of models had uncovered a potential new pathway for cancer therapy — one that could help “cold” tumours become visible to the immune system.
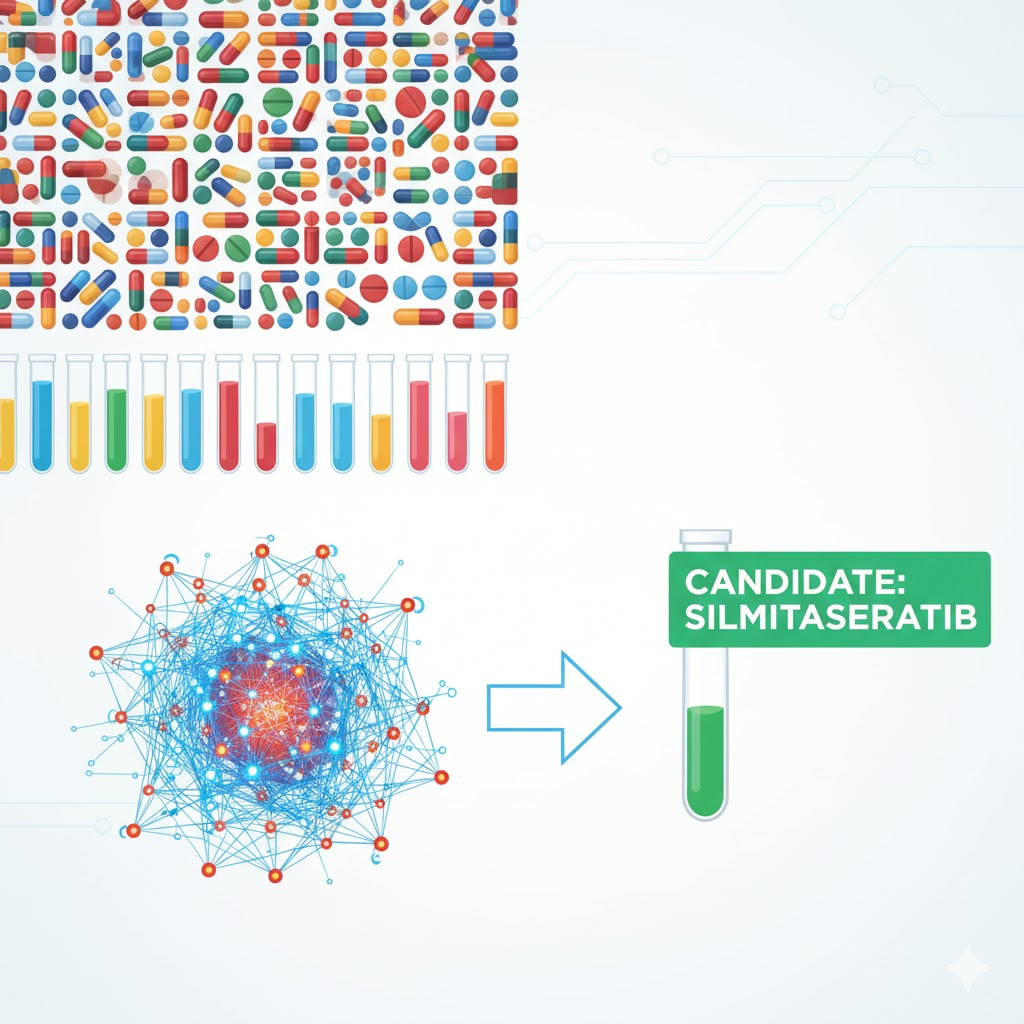
This wasn’t just data analysis — it was true scientific discovery. The AI model, C2S-Scale 27B, built on the Gemma architecture, analyzed thousands of drug interactions and predicted a novel combination: Silmitasertib (a CK2 inhibitor) plus low-dose interferon. Together, these could improve how tumour cells present antigens to immune cells.
Decrypt’s coverage called it “a glimpse into the future of medical AI.” The model didn’t just confirm what scientists already knew — it generated a hypothesis later proven in laboratory experiments.
The Gemma model cancer therapy pathway could redefine how we discover drugs, test treatments, and personalize care in the years to come.
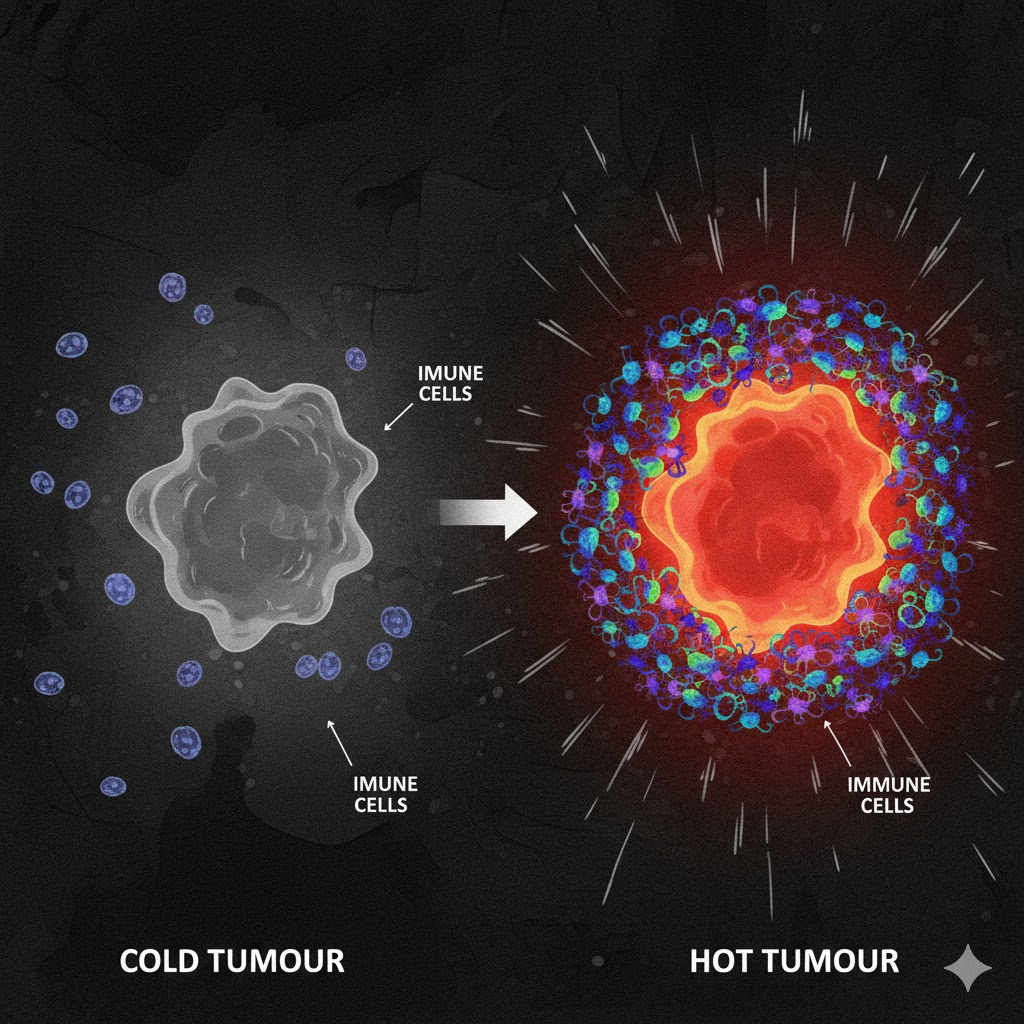
The Problem: Cold Tumours and Immune Invisibility
The Gemma model cancer therapy pathway tackles a fundamental issue in oncology — cold tumours that evade immune detection.
In immunotherapy, success depends on whether the immune system can “see” cancer cells. Many tumours hide by reducing antigen presentation, the process that signals danger to immune cells.
As noted by Google’s AI team, this invisibility makes them resistant to modern immune-based treatments.
The Gemma-based model simulated thousands of drug interactions in two cellular contexts:
- Immune-context positive: where tumour-immune signals existed
- Immune-context neutral: where no immune cues were present
This contextual comparison helped the AI pinpoint drugs that boosted immune visibility only in the right environment. Such precision is what made the Gemma model cancer therapy pathway stand out.
The Decoder’s analysis highlighted that this method could lead to breakthroughs in other immune-based diseases too.
How the Gemma Model Made the Discovery
To uncover the Gemma model cancer therapy pathway, scientists created C2S-Scale 27B, a 27-billion parameter model capable of understanding cellular communication like language.
It analyzed massive single-cell datasets, simulating more than 4,000 drugs across two immune environments. The model sought drugs that worked conditionally — effective only when immune context existed.
Out of all tested compounds, it identified Silmitasertib — previously known for treating certain tumours — as a promising candidate. When combined with interferon, the model predicted improved antigen presentation, a critical factor in immune recognition.
When researchers later validated this in the lab, results matched perfectly. As Investing.com reported, the AI had essentially made a real biological discovery — something scientists traditionally take years to accomplish.
This model doesn’t just interpret data; it creates hypotheses that can be tested in real-world biology.
From Simulation to the Lab: Real-World Validation
The Gemma model cancer therapy pathway moved from virtual simulation to laboratory validation — a crucial step in proving AI’s scientific credibility.
In lab tests, tumour cells were treated with Silmitasertib alone, interferon alone, and the combination. Neither drug alone made a major difference. Together, they increased MHC Class I antigen presentation by nearly 50%.
According to Google’s AI blog, this combination made “cold” tumour cells more visible to immune cells, confirming the model’s prediction.
This result shows AI’s potential to predict context-dependent drug synergies, helping researchers explore thousands of possible combinations before conducting costly lab work.
The Decoder emphasized that this could shorten drug discovery cycles from years to months.
For the first time, a machine learning model didn’t just process data — it pointed scientists toward a real-world therapeutic pathway.
Why This Is a Milestone in AI and Medicine
The Gemma model cancer therapy pathway demonstrates how artificial intelligence can become a true research partner in medicine.
Unlike older models that merely recognized data patterns, the Gemma architecture showed emergent reasoning — it understood the why behind biological interactions.
As the Decrypt article explained, this is “the first time a large model suggested a combination that worked conditionally in a biological setting.”
Three reasons make this a milestone:
- Scale – 27 billion parameters enable deep cellular understanding.
- Contextual intelligence – Ability to reason about immune environments.
- Open access – Researchers can freely explore or build upon it via Google’s open Gemma models.
This AI isn’t replacing scientists — it’s empowering them. The Gemma model cancer therapy pathway proves AI can be a co-researcher, capable of suggesting truly novel ideas.

What It Means for Cancer Research and Patients
The Gemma model cancer therapy pathway offers hope for patients and guidance for researchers.
For scientists, it means a faster way to identify promising drug combinations and study immune mechanisms at scale. For clinicians, it may one day help predict which patients will respond to specific immunotherapies.
Investing.com noted that such discoveries can accelerate early-stage cancer research and drug testing dramatically.
Still, experts caution that the results are pre-clinical — verified in vitro, not yet in humans. As Google’s official statement said: “With further research and trials, this may represent a new therapeutic pathway.”
For now, it signals a shift from AI as an assistant to AI as a biological collaborator — one that doesn’t just find answers but creates new questions worth asking.

The Future and Final Thoughts
The Gemma model cancer therapy pathway might be remembered as the start of AI-driven drug discovery.
Its real breakthrough isn’t just identifying Silmitasertib’s hidden potential — it’s proving that AI can create scientific knowledge. That’s a new chapter in research.
The Decoder wrote that “this sets a new bar for what AI–biology collaborations can achieve.”
Google’s open-source move ensures labs worldwide can validate and expand the finding. It’s a democratization of discovery — anyone with curiosity and data can participate.
The next version of the Gemma model may explore how similar pathways could help with autoimmune diseases or viral infections.
As science and AI converge, the Gemma model cancer therapy pathway stands as a reminder that technology doesn’t just automate — it illuminates.
AI didn’t just find correlations this time; it found a potential cure pathway — and that’s revolutionary.

Comments